——————————————————————————————————————
December 2014 – http://www.fda.gov/womens
The FDA has just issued a warning on ultrasound. If you follow the links, you will see this is a warning for non-ionizing radiation due to potential tissue heating. ALARA (As Low As Reasonably Achievable) is called for. See link and notice below: http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm095508.htm
Ultrasound Imaging
Ultrasound imaging is the most widely used medical imaging method during pregnancy. Fetal ultrasound imaging provides real-time images of the fetus. Doppler fetal ultrasound heartbeat monitors are hand-held ultrasound devices that let you listen to the heartbeat of the fetus. Both are prescription devices designed to be used by trained health care professionals.
The FDA discourages fetal imaging for keepsake videos and other non-medical purposes. The FDA is concerned about over-the-counter sale of prescription fetal ultrasound heartbeat monitors (also called doptones). These devices, when used by untrained persons, could expose the fetus to prolonged and unsafe energy levels or could provide information that is interpreted incorrectly.
- View FDA’s new Ultrasound Webpage
- Share the consumer update: Avoid Fetal “Keepsake” Images, Heartbeat Monitors
——————————————————————————————————————
MRI (Magnetic Resonance Imaging)
http://ms.about.com/od/multiplesclerosis101/f/mri_radiation.htm
http://www.diffen.com/difference/CT_Scan_vs_MRI
——————————————————————————————————————
Prolonged exposure to low doses of radiation ups cancer risk—study
October 22nd, 2015
PARIS, France—Prolonged exposure to even low doses of radiation increases the risk of cancer, according to a new study of workers in the nuclear sector in Britain, France and the United States.
The results, published Wednesday in the British Medical Journal, provides “direct evidence about cancer risks after protracted exposures to low-dose ionizing radiation,” said the International Agency for Research on Cancer (IARC), the cancer agency of the World Health Organization, which coordinated the study.
The findings demonstrate “a significant association between increasing radiation dose and risk of all solid cancers,” said the study’s co-author IARC researcher Dr Ausrele Kesminiene.
“No matter whether people are exposed to protracted low doses or to high and acute doses, the observed association between dose and solid cancer risk is similar per unit of radiation dose,” he added.
The International Nuclear Workers Study (INWORKS), a collaboration between international partners, evaluated the exposures of more than 300,000 nuclear workers in Britain, France and the United States between 1943 and 2005.
The results showed that the risk of death from solid cancers was “modest” but that one in every hundred cancer deaths could be attributed to workplace radiation exposure.
“The findings are important not only for the protection of workers in the nuclear industry but also for medical staff and the general population,” since the level of doses received by nuclear workers is comparable with that received by patients repeatedly exposed to CT scans or other radiology procedures, said IARC researcher Dr Isabelle Thierry-Chef.
“This stresses the importance of striking a balance between the risks and the benefits of such medical imaging procedures,” she added.
The average age of workers in the study was 58 years.
——————————————————————————————————————
How Much Do CT Scans Increase the Risk of Cancer?
Researchers reevaluate the safety of radiation used in medical imaging
Jun 18, 2013 |By Carina Storrs
Ever since physicians started regularly ordering CT (computed tomography) scans four decades ago, researchers have worried that the medical imaging procedure could increase a patient’s risk of developing cancer. CT scanners bombard the human body with x-ray beams, which can damage DNA and create mutations that spur cells to grow into tumors.
Doctors have always assumed, however, that the benefits outweigh the risks. The x-rays, which rotate around the head, chest or another body part, help to create a three-dimensional image that is much more detailed than pictures from a standard x-ray machine. But a single CT scan subjects the human body to between 150 and 1,100 times the radiation of a conventional x-ray, or around a year’s worth of exposure to radiation from both natural and artificial sources in the environment.
A handful of studies published in the past decade have rekindled concerns. Researchers at the National Cancer Institute estimate that 29,000 future cancer cases could be attributed to the 72 million CT scans performed in the country in 2007. That increase is equivalent to about 2 percent of the total 1.7 million cancers diagnosed nationwide every year. A 2009 study of medical centers in the San Francisco Bay Area also calculated an elevated risk: one extra case of cancer for every 400 to 2,000 routine chest CT exams.
The reliability of such predictions depends, of course, on how scientists measure the underlying link between radiation and cancer in the first place. In fact, most estimates of the excess cancer risk from CT scans over the past several decades rely largely on a potentially misleading data set: cancer rates among the long-term survivors of the atomic bomb blasts in World War II.
“There are major concerns with taking the atomic bomb survivor data and trying to understand what the risk might be to people exposed to CT scans,” says David Richardson, an associate professor of epidemiology at the University of North Carolina Gillings School of Global Public Health who has done research on the atomic bomb survivors.
About 25,000 atomic bomb survivors were exposed to relatively low doses of radiation comparable to between one and three CT scans. The number of cancer cases that developed over the rest of their lives is not, however, large enough to provide the necessary statistical power to reliably predict the cancer risk associated with CT scans in the general population today. Given these difficulties, as well as renewed concerns about radiation levels and the lack of mandatory standards for safe CT exposure (in contrast to such procedures as mammography), a dozen groups of investigators around the world have decided to reevaluate the risk of CT radiation based on more complete evidence.
A growing number of clinicians and medical associations are not waiting for definitive results about health risks and have already begun figuring out how to reduce radiation levels. Two radiologists at Massachusetts General Hospital, for example, think that they can decrease the x-ray dosage of at least one common type of CT scan by 75 percent without significantly reducing image quality. Likewise, a few medical associations are trying to limit superfluous imaging and prevent clinicians from using too much radiation when CT scanning is necessary.
Outdated Data
For obvious ethical reasons, researchers cannot irradiate people solely to estimate the cancer risk of CT. So scientists turned to data about survivors of the atomic bombs dropped on Hiroshima and Nagasaki in August 1945. Between 150,000 and 200,000 people died during the detonations and in the months following them. Most individuals within one kilometer of the bombings perished from acute radiation poisoning, falling debris or fires that erupted in the immediate aftermath of the attack. Some people within 2.5 kilometers of ground zero lived for years after exposure to varying levels of gamma rays, from a high end of more than three sieverts (Sv)—which can burn skin and cause hair loss—to a low end of five millisieverts (mSv), which is in the middle of the typical range for CT scans today (2 to 10 mSv). A sievert is an international unit for measuring the effects of different kinds of radiation on living tissue: 1 Sv of gamma rays causes the same amount of tissue damage as 1 Sv of x-rays.
Several years after the blasts, researchers began tracking rates of disease and death among more than 120,000 survivors. The results demonstrated, for the first time, that the cancer risk from radiation depends on the dose and that even very small doses can up the odds. Based on such data, a 2006 report from the National Research Council has estimated that exposure to 10 mSv—the approximate dose from a CT scan of the abdomen—increases the lifetime risk of developing any cancer by 0.1 percent. Using the same basic information, the U.S. Food and Drug Administration concluded that 10 mSv increases the risk of a fatal cancer by 0.05 percent. Because these risks are tiny compared with the natural incidence of cancer in the general population, they do not seem alarming. Any one person in the U.S. has a 20 percent chance of dying from cancer. Therefore, a single CT scan increases the average patient’s risk of developing a fatal tumor from 20 to 20.05 percent.
All these estimates share a serious flaw. Among survivors exposed to 100 mSv of radiation or less—including the doses typical for CT scans—the numbers of cancer cases and deaths are so small that it becomes virtually impossible to be certain that they are significantly higher than the rate of cancer in the general population. To compensate, the National Research Council and others based their estimates primarily on data from survivors who were exposed to levels of radiation in the range of 100 mSv to 2 Sv. The fundamental assumption is that cancer risk and radiation dose have a similar relationship in high and low ranges—but that is not necessarily true.
Another complicating factor is that the atomic bombs exposed people’s entire body to one large blast of gamma rays, whereas many patients receive multiple CT scans that concentrate several x-rays on one region of their body, making accurate comparisons tricky. Compounding this issue, the atomic bomb survivors typically had much poorer nutrition and less access to medical care compared with today’s general U.S. population. Thus, the same level of radiation might correspond to greater illness in an atomic bomb survivor than in an otherwise healthy person from today.
Dialing Down the Dose
To conclusively determine the risk of low radiation doses and set new safety standards for CT radiation, researchers are beginning to abandon the atomic bomb survivor data and directly investigate the number of cancers among people who have received CT scans. About a dozen such studies from different countries examining rates of various cancers following CT scans will be published in the next few years.
In the meantime, some researchers have started testing whether good images can be produced with radiation doses lower than those generated in typical CT scans. Sarabjeet Singh, a radiologist at Mass General, and his fellow radiologist Mannudeep Kalra have an unusual way of conducting such investigations. Rather than recruiting living, breathing human volunteers for their studies, they work with cadavers. In that way, they can scan bodies many times without worrying about making people sick and can perform an autopsy to check whether the scan has correctly identified a medical problem.
So far the researchers have discovered that they can diagnose certain abnormal growths in the lungs and perform routine chest exams with about 75 percent less radiation than usual—a strategy Mass General has since adopted. Singh and Kalra are now sharing their methods with radiologists and technologists from hospitals and scanning centers across the U.S. and around the globe.
Medical associations are stepping in to help as well. Because the FDA does not regulate how CT scanners are used or set dose limits, different centers end up using an array of radiation doses—some of which seem unnecessarily high. In the past year the American Association of Physicists in Medicine has rolled out standardized procedures for adult CT exams that should rein in some of these outlier centers, Singh says. Furthermore, an increasing number of CT facilities across the U.S. receive accreditation from the American College of Radiology, which sets limits for radiation doses and evaluates image quality. In 2012 accreditation became mandatory for outpatient clinics that accept Medicare Part B if the facilities want to get reimbursed for scans.
No matter how much clinicians lower the levels of radiation used in individual CT exams, however, a problem remains. Many people still receive unnecessary CT scans and, along with them, unneeded doses of radiation. Bruce Hillman of the University of Virginia and other researchers worry that emergency room physicians in particular order too many CT scans, making quick decisions in high-pressure situations. In a 2004 poll 91 percent of ER doctors did not think a CT scan posed any cancer risk. Doctors and their patients may finally be getting the message. A 2012 analysis of Medicare data suggests that the previously rampant growth in CT procedures is flattening out and possibly waning.
“The jury is still out on whether there is a small cancer risk,” says Donald Frush, chief of pediatric radiology at Duke University Medical Center. “But the safest thing is to assume that no amount of radiation is safe. And if we find out in 20 years that a little bit was not harmful, then what did we lose by trying to minimize the dose?”
http://www.scientificamerican.com/article/how-much-ct-scans-increase-risk-cancer/
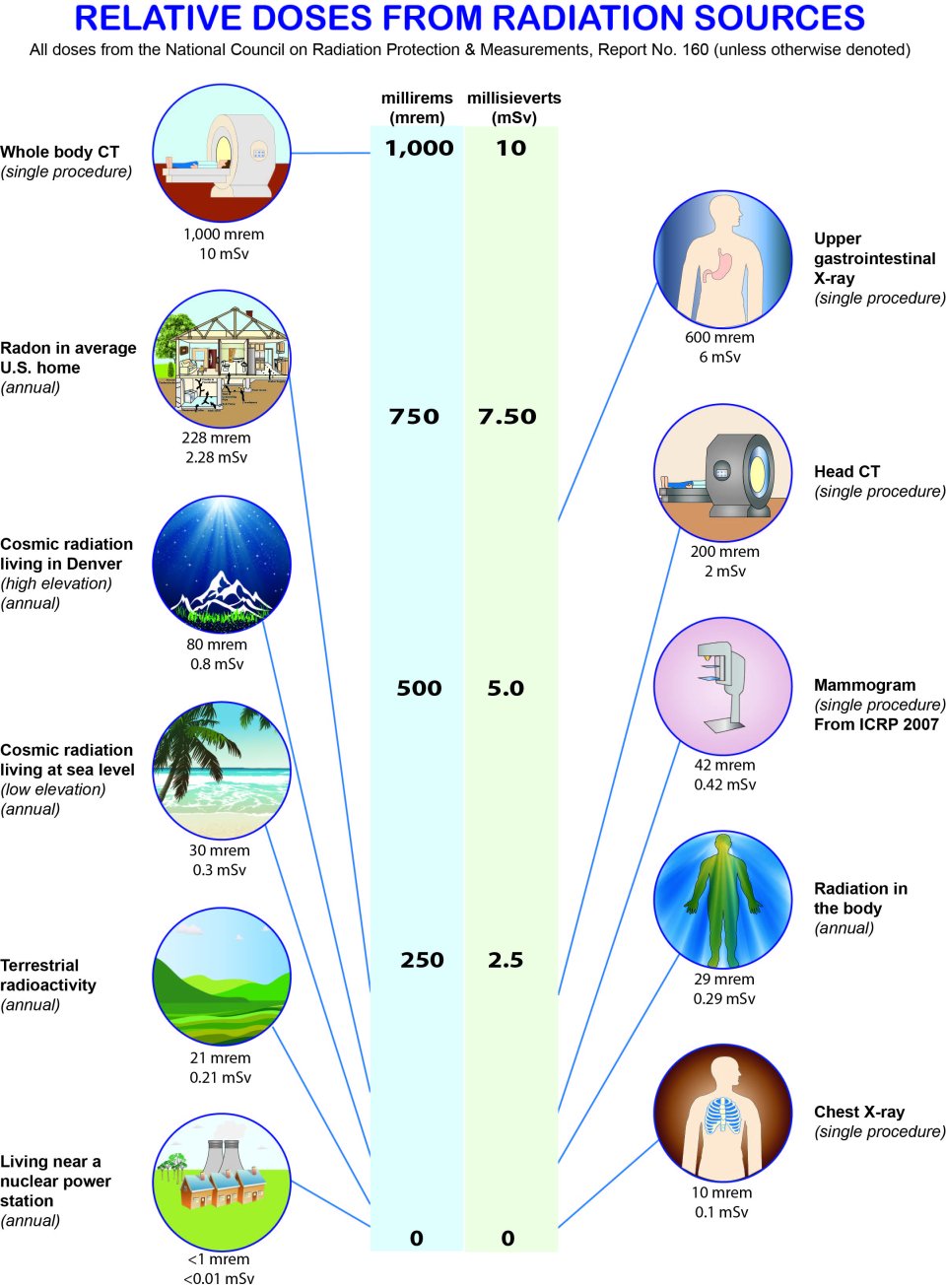
source : https://www.epa.gov/radiation/radiation-sources-and-doses#tab-2
——————————————————————————————————————
Calculate your Exposure
http://www.rfwireless-world.com/calculators/RF-exposure-calculator.html
http://hintlink.com/power_density.htm
http://www.xrayrisk.com/calculator/calculator.php
——————————————————————————————————————
Nurse with rare brain disorder wins $4M suit against hospital
November 23, 2014 | 6:58am
A Manhattan nurse practitioner with a rare brain disorder won a $4 million judgment last week against New York Presbyterian Hospital — seven years after she sued the hospital for forcing her to work in units that exacerbated her painful condition.
Rebecca Serdans, 48, has dystonia, a neurological condition that impairs mobility. In 2004, doctors implanted a deep brain stimulator in her head to ease the symptoms.
Electromagnetic waves — abundant at New York Presbyterian, where Serdans worked — disrupt the effectiveness of the device.
Serdans was able to work in the hospital’s Cardio-Thoracic Intensive Care Unit — where her device functioned without incident, she said.
But in 2007, she was switched to another unit, where her brain implant failed, leaving her in pain after a single shift and forcing her to get the device reprogrammed, she claimed.
“They knew what they were doing,” she said of the hospital.
She says the hospital stopped calling her in to work after she complained and asked to be transferred to a different area.
Serdans sued in 2008 and was won the $4 million judgment last week.
“We believe the verdict has no legal or factual basis and intend to appeal,” a hospital spokesperson said.
“This is a hospital worth $4 billion,” said her attorney, Derek Smith. “You would think that a hospital with a reputation for taking care of its patients would also take care of its employees.”
http://nypost.com/2014/11/23/nurse-with-rare-brain-disorder-wins-4m-suit-against-hospital/
——————————————————————————————————————
Wireless Monitors
Hospitals have various machines that patients are attached to, some use wireless networks.
Private wireless networks monitor the machines and the patient and sends data wirelessly.
Here is an example of one brand used in Canada.
“…Alaris® Asset Management and the Stanley Healthcare AeroScout Real-Time Location System
Wirelessly manage device inventory and utilization Alaris® Asset Management and the Stanley Healthcare AeroScout RTLS help you more efficiently manage Alaris infusion device inventory and utilization. Leveraging your existing Wi-Fi network, the solution quickly helps locate the available Alaris infusion devices and optimize your overall device utilization.”
http://www.carefusion-products.com/assets/supportdocs/DFUs/1000DF00327.pdf
Operating Precautions (continued) Electromagnetic Compatibility and Interference
This pump is protected against the effects of external interference, including high energy radio frequency emissions, magnetic fields and electrostatic discharge (for example, as generated by electrosurgical and cauterising equipment, large motors, portable radios, cellular telephones etc.) and is designed to remain safe when unreasonable levels of interference are encountered.
Therapeutic Radiation Equipment: Do not use the pump in the vicinity of any Therapeutic Radiation Equipment. Levels of radiation generated by the radiation therapy equipment such as Linear Accelerator, may severely affect functioning of the pump. Please consult manufacturer’s recommendations for safe distance and other precautionary requirements. For further information, please contact your local CareFusion representative.
Magnetic Resonance Imaging (MRI): The pump contains ferromagnetic materials which are susceptible to interference with magnetic field generated by the MRI devices. Therefore, the pump is not considered an MRI compatible pump as such. If use of the pump within an MRI environment is unavoidable, then CareFusion highly recommends securing the pump at a safe distance from the magnetic field outside the identified ‘Controlled Access Area’ in order to evade any magnetic interference to the pump; or MRI image distortion. This safe distance should be established in accordance with the manufacturers’ recommendations regarding electromagnetic interference (EMI). For further information, please refer to the product technical service manual (TSM). Alternatively, contact your local CareFusion representative for further guidance.
Accessories: Do not use any non-recommended accessory with the pump. The pump is tested and compliant with the relevant EMC claims only with the recommended accessories. Use of any accessory, transducer or cable other than those specified by CareFusion may result in increased emissions or decreased pump immunity.
This pump is a CISPR 11 Group 1 Class A device and uses RF energy only for its internal function in the normal product offering. Therefore, its RF emissions are very low and are not likely to cause any interference with the nearby electronic equipment. However, this pump emits a certain level of electromagnetic radiation which is within the levels specified by IEC/EN60601-1-2 and IEC/EN60601-2-24. If the pump interacts with other equipment, measures should be taken to minimise the effects, for instance by repositioning or relocation.
In some circumstances the pump may be affected by an electrostatic discharge through air at levels close to or above 15kv; or by radio frequency radiation close to or above 10v/m. If the pump is affected by this external interference the pump will remain in a safe mode; the pump will duly stop the infusion and alert the user by generating a combination of visual and audible alarms. Should any encountered alarm condition persist even after user intervention, it is recommended to replace that particular pump and quarantine the pump for the attention of appropriately trained technical personnel. (Consult Technical Service Manual for further information).”
Wireless Medical Telemetry Service (WMTS)
608 – 614, 1395 – 1400, and 1427 – 1432 MHz range
https://www.fcc.gov/encyclopedia/wireless-medical-telemetry-service-wmts
http://www.google.com/patents/US8038593
——————————————————————————————————————
Wireless Implants
RFID in medical devices is a concern also since it would be long term exposure. Here are some links related to the subject :
Medical Device Radiocommunications Service (MedRadio)
401 – 406, 413 – 419, 426 – 432, 438 – 444, and 451 – 457 MHz range
www.fcc.gov/encyclopedia/medical-device-radiocommunications-service-medradio
——————————————————————————————————————
Study of Electromagnetic Risk Analysis in Hospitals
http://ece-events.unm.edu/amerem2014/Resources/taggedABSTRACTS/155.pdf
Radiation Risk of Medical Imaging for Adults and Children
http://www.insideradiology.com.au/pages/view.php?T_id=57#.V_y5tumd6Zw